



Lowering of the genitals
What is pelvic organ prolapse?
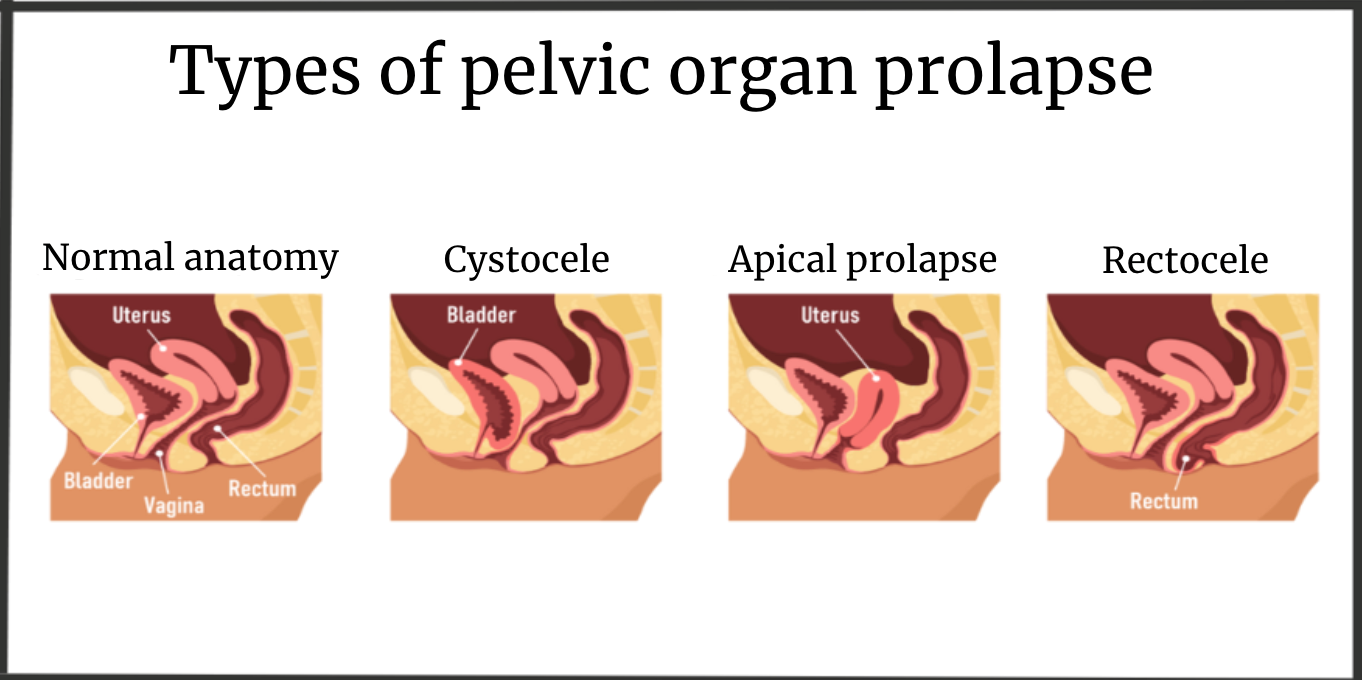
Pelvic organ prolapse, or prolapse, occurs when the muscles and ligaments supporting the pelvic organs become weakened or stretched. This can lead to displacement or prolapse of the uterus, bladder, or rectum. This condition can cause discomfort, pain, and problems with urination or bowel movements.
Prolapse of the vaginal walls and uterus, as well as the prolapse of the vaginal walls and uterus, is a very common issue in women. Unfortunately, about 30% of women suffer from this, and approximately 10-15% of women suffer to such an extent that surgical intervention is necessary to solve the problem, despite a wide range of non-surgical methods, such as pessary insertion, Kegel exercises, and aesthetic gynecology techniques.
In the illustration below, different stages of uterine prolapse are shown schematically:
Indications for Surgical Treatment
The decision to perform surgery for pelvic organ prolapse in women is not always straightforward. Certainly, the more pronounced the degree of prolapse, the higher the chance that a woman will want surgery, and surgery is often the preferred method in such cases. However, sometimes we still recommend pessaries (more often in older women) even in significant prolapse, and occasionally we perform surgery even for mild prolapse (more often in younger women).
Today, there are about 200 surgical procedures for pelvic organ prolapse and urinary incontinence in women. In real practice, there are about 20 different surgeries performed via vaginal or laparoscopic approaches. Each of these surgeries has different indications and contraindications, so the final decision on whether you need surgery, and if so, which one, can only be made during a consultation. Please note that for consultations regarding pelvic organ prolapse and urinary incontinence, it is important to come with a full bladder.
Preparation for the Procedure
Before the procedure, several tests are needed to assess overall health:
- Complete blood count with leukocyte formula
- Biochemical blood test
- Rh factor and blood type
- Coagulogram
- Blood glucose
- General urinalysis
- Consultation with a therapist + ECG, dentist consultation (to exclude any loose teeth)
- Chest X-ray (if the previous one was done a year ago)
- Consultation with relevant specialists if there are chronic diseases (e.g., endocrinologist for diabetes, pulmonologist for asthma, etc.)
Anesthesia Methods for Classic TVT-o Surgeries:
- Intravenous anesthesia (with tracheal intubation)
- Spinal anesthesia (SMA)
Hospital Stay Duration: 2-3 days
Postoperative Period
- Typically, the patient gets out of bed 3-4 hours after surgery.
- Eating and drinking can begin on the day of surgery.
- Normal lifestyle resumes the next day with limitations on physical activity (sports) for 2-3 weeks.
- Sexual activity can be resumed 1-1.5 months after surgery.
- No dressings are required.
- Follow-up examination after 1.5 months.
What is Normal After This Surgery:
- Moderate discomfort in the perineum, during urination.
- A slight increase in body temperature up to 37.5°C, sometimes higher, especially if the temperature only rises in the evening and is managed by paracetamol 500-1000 mg.
- Slight abdominal bloating, constipation, or diarrhea in the first days after surgery.
- Mild weakness, drowsiness.
- Bloody vaginal discharge for several days to 3 weeks after surgery.
We have the most extensive experience in performing pelvic organ prolapse surgeries in the Chernihiv region and will use the method that best suits your needs.
We will discuss all questions regarding the surgery and the postoperative period during our meeting at the clinic.
You can view these and other surgeries on my YouTube channel.