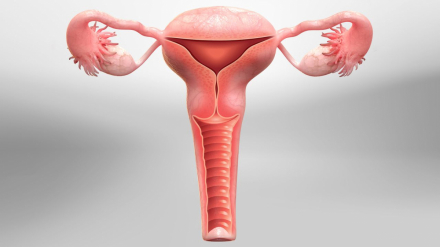




Correction of prolapse of the uterus and vaginal walls
Prolapse of the vaginal walls and uterus is a very common issue for women. On average, 10-12% of women will need surgical treatment for this problem during their lifetime. More than 200 different surgical procedures for the treatment of genital prolapse in women have been described in the literature. At present, 15-20 relatively standardized operations remain.
Why are there so many procedures? Unfortunately, this is due to the complexity of the ligamentous and fascial apparatus that supports the female reproductive organs in their normal position and the functional anatomy of these organs. Female reproductive organs are not static but actively move and change shape in various life situations. They are constantly "collaborating" with adjacent organs (the bladder and rectum), which are in direct contact. As a result, there is no single surgery that is 100% suitable for every patient.
Modern surgery largely takes into account these anatomical features and replaces structures that have lost their supporting function either partially or completely.
Currently, there are 5 main procedures and their modifications that are still relevant:
- High sacro-uterine ligament plication (via laparoscopic or vaginal approach)
- Promontofixation (sacral colpopexy)
- Pectopexy and lateral fixation
- Sacrospinous colpopexy (using native tissue or a mesh endoprosthesis)
- Lateral aponeurotic mesh vaginopexy of the uterus
Is it necessary to remove the uterus?
No, removing the uterus is not mandatory in prolapse surgery!
What are the symptoms of pelvic organ prolapse? Mild uterine prolapse often occurs after childbirth and usually does not cause any symptoms. Symptoms of moderate to severe prolapse include:
- Feeling and/or noticing the vaginal walls protruding outward
- A feeling of heaviness or discomfort in the lower abdomen
- Feeling incomplete emptying of the bladder
- Urinary incontinence
- Problems with bowel movements and the need to press on the vagina to assist with defecation
- The sensation of sitting on a small ball
- A feeling that the vaginal walls are rubbing against clothing
- Lower back pain
What preoperative preparations and tests are necessary? You need to undergo a series of tests, including:
- Complete blood count with differential
- Blood chemistry
- Blood type and Rh factor
- Coagulation profile
- Blood glucose level
- Urinalysis
- Therapist consultation + ECG, dentist consultation (to exclude loose teeth)
- Chest X-ray (if the previous one was done more than a year ago)
- Consultations with relevant specialists if you have chronic conditions (for example, an endocrinologist for diabetes or a pulmonologist for asthma)
All these tests can be done at our clinic.
There are no dietary or fluid restrictions the day before surgery. After midnight before surgery, avoid eating and drinking. Bowel preparation with an enema or special medications is not required.
We will also discuss any medications you are taking and whether you should continue or stop them before surgery.
Postoperative recovery:
- Patients typically get out of bed 3-4 hours after surgery
- You can start eating light food and drinking fluids a few hours after surgery
- Dressings are changed daily until discharge (the vaginal pack is removed 12-24 hours post-op)
- You can shower the day after surgery, and take a bath after 3-4 weeks
- Physical activities such as sports, swimming, or running should be limited for up to 4 weeks, but you can return to your normal life
- Sexual activity should be avoided for 1.5-2 months
- A follow-up visit, if no complications, is usually recommended in 2-3 months
What is normal after laparoscopic prolapse surgery?
- Mild discomfort in the perineal area
- Slight fever up to 37.5°C (99.5°F), sometimes higher, especially in the evening, which can be reduced with paracetamol (500-1000 mg)
- Mild bloating, constipation, or diarrhea in the first days after surgery
- Slight weakness and sleepiness
- Blood discharge from the vagina for a few days to 4-6 weeks post-op. Use pads, not tampons, for any bleeding.
- Pain in the chest area, especially on the right side and near the right clavicle (this is a consequence of carbon dioxide pressure during laparoscopy). It is harmless and typically resolves within 2-3 days.
We will discuss all questions about the surgery and postoperative period during your consultation at the clinic.
You can view these and other surgeries on my YouTube channel.